

Typically making its unwelcome arrival during puberty, acne ranges from small whiteheads to painful cystic lesions. Over-the-counter medications usually contain astringents, agents that help to dry out oily skin. Active ingredients include witch hazel, rubbing alcohol, or even salicylic acid. Astringents work by removing oil and unclogging the skin’s pores. More recently, medications with adapalene (a retinoid similar to prescription Retin-A) and benzoyl peroxide (an antiseptic that eliminates germs on the skin) have been made available without a prescription. While using these topical medications does not require a doctor’s order, it’s important to discuss their use with a trusted health professional. Adapalene can cause dryness and redness of the skin and can make the user more prone to sunburn. Benzoyl peroxide is safe to use on skin, but will likely bleach any fabrics it contacts, including towels and sheets.
Prescription medications build on these, but add topical antibiotics, like Clindamycin, which specifically targets the germ that causes acne. If these fail, doctors can suggest certain oral antibiotics (like minocycline or doxycycline). In females, if the timing of breakouts is related to the menstrual cycle, taking birth control pills might help. If the acne is painful, cystic, or if it’s leaving scars behind, a dermatologist might recommend Accutane, a prescription medication that is reserved for the most severe cases of acne. While generally safe, Accutane can cause changes in liver function tests and severe birth defects should the patient get pregnant while taking it. Very close medical supervision is required for this prescription.
In general, eating a healthy diet, drinking plenty of water, and keeping the skin clean are great ways to practice good skin hygiene.

First-degree burns look red, like a simple sunburn, and rarely cause permanent damage. Second-degree burns develop blisters, but still often heal without scarring. Third- and Fourth-degree burns cause serious damage to the deeper layers of the skin and can even require surgical repair and skin grafting. Full-thickness tissue damage can even lead to motor disability if muscles and joints are involved. Degree of heat, duration of exposure, body surface area affected, and mechanism of injury all contribute to severity of skin damage. The first thing to do with a burn is remove the source of the heat. Next, application of cold water will help reverse the thermal injury and halt further damage.
To protect younger children, make sure the handles of pots and pans on the stove face inward and don’t hang over the edge of the counter as a temptation for curious toddlers. For 9-month-olds who are learning to pull up to standing position, a tablecloth might look like a good thing to grab onto for support. If there’s a steaming mug of tea of coffee on the table, it could spill on the child if the tablecloth is pulled. To reduce the risk of burns, The American Academy of Pediatrics recommends that a home’s hot water heater be set to a maximum temperature of 120 degrees F. Stoves, space heaters, grills, fire pits, and radiators can be dangerous, and children should be educated and supervised to avoid these. Steamers, clothing irons, and curling irons should be kept out of reach and only used by an adult. In homes with younger children, all wall outlets should have plug-covers inserted to reduce the risk of electrical burn. As always, apply sunscreen liberally when outside during the warmer months.

Fifth Disease, also known as Erythema Infectiosum, also known as Slapped Cheek, is a viral infection caused by Parvovirus-B19. It’s one of the most common rashes in children, typically presenting in younger age groups in the Spring and Summer months. It’s designation comes from it being the fifth rash to be described, after Measles, Roseola, Chicken Pox, and Rubella. Typically this rash presents as a triangular-shaped smooth red patch of skin on the cheeks. This might be accompanied by mild fever and runny nose. As this rash fades, the child usually develops a lacy red pattern on the trunk and extremities, which can last up to three weeks.
Parvovirus infection is harmless for most everyone, but patients with Sickle Cell Anemia can have a more severe response to this viral infection. Similarly, patients with underlying hemolytic anemia can get quite ill from Parvovirus. Lastly, women in their first trimester of pregnancy who have never had Parvovirus before can potentially suffer fetal damage from this germ. Because this infection takes some time to manifest, usually by the time the rash is visible, the patient has already been infected for a while, and is no longer contagious. In general, avoidance of viral infections can be bolstered by good hand-washing and responsible management of respiratory droplets (sneezing into the elbow, using tissues instead of sleeves).

Also known as Hand, Foot, and Mouth disease, this viral infection is typically seen in preschool-aged children in the late Summer and early Fall months. The virus is named for Coxsackie, New York, the town where it was first reported in the 1940s. Symptoms often include blistering lesions on the extremities and in and around the mouth. Lesions can look like red bumps on the soles of the feet and palms of the hands, or a similar-looking rash on the lower face. It can even cause frank blistering of the skin, often in-between fingers or toes. In the mouth, we find evidence of this infection on the tongue and in the very back of the throat. This can make it uncomfortable or even painful to eat and drink, particularly if the food is acidic (like fruit juice). While this germ sometimes comes with a fever, the small portion of children who are hospitalized with Coxsackievirus are often go to the Emergency Room for dehydration, because their oral lesions make drinking difficult or painful.
Don’t confuse this human germ with cattle’s Hoof and Mouth disease. These viruses don’t cross from one species to another. Going to a petting zoo is not a risk factor for contracting Hand Foot and Mouth. It is spread, like so many other viruses, through respiratory droplets from one person to another. Prevention, then, relies on attention to hygiene, including covering sneezes properly and frequent hand washing.

The name can be misleading since no worms are involved with this infection. The lesion itself often appears to have a flat, dry center with a heaped-up circumference that can look like a coiled worm. On the skin, we call this tinea corporis. It is contracted through direct contact with an infected person or a surface they touched. Commonly, this includes a wrestling mat, poolside floor, shared wearable sporting equipment, or a towel. It is usually treated with a topical antifungal over the course of several weeks, with full resolution. Rarely do these lesions leave a scar. On the scalp, we call this tinea capitis, and it’s a little trickier to treat. Because the available topical treatments don’t have optimal absorption through the scalp, we prescribe an oral antifungal when these lesions cross the hairline. Even though this medication has a 6-8 week course, kids often don’t mind taking it. It gets absorbed better when administered with a fatty food, so kids will get a cookie and whole milk or another treat, making it less of a struggle than some other courses of medication.
Scalp lesions might be seen after a haircut if the barber’s trimmers weren’t sanitized properly, or parents might notice lymph nodes in the neck, a sign of the body’s immune system trying to fight off this germ. Or, the first indication of a tinea infection can be hair loss. Specifically within the circular outline of this lesion, the hair often doesn’t grow. Once the infection is fully treated, the hair grows back as usual.
Person-to-person spread can be reduced by sanitizing gym equipment between uses, not sharing towels, and generally keeping one’s hands clean by using soap and water regularly.

Classic impetigo looks like “honey crusted” lesions, often around orifices like the nose or mouth, but can occur anywhere. Usually it begins with an insult to the skin that compromises the skin’s barrier, like a scratch or pimple. Germs get into this space and cause a shallow skin infection. Usually all that’s needed to treat impetigo is a topical prescription antibiotic ointment. Sometimes, however, impetigo blisters up, and it’s then designated bullous impetigo. This version of impetigo might need an oral antibiotic to resolve.
Contagion is usually skin-to-skin, when contact is made with an infected individual. Prevention measures include making sure the skin (your best protective barrier) is intact and the healthy. Frequent hand washing is also helpful.
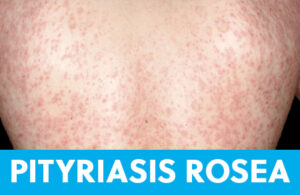
Also known as the Christmas-tree rash, this is a self-limiting eruption that can last for months. Its nickname comes from the orientation of lesions that are oval-shaped with the long axis pointing upwards toward the midline of the back and downward toward the patient’s hips. Sometimes the rash wraps around the front of the torso and this pattern continues. There is often a “herald patch”, a larger lesion usually on the lower abdomen or thigh that precedes the more diffuse rash. Regular readers of this series might notice that the herald patch looks familiar. Out of context, this lesion can look quite a bit like tinea corporis (ringworm). Pityriasis rosea lesions are flat and have a “collarette” (or ring) of fine scale on their periphery. Patients might complain of itching, but often the only symptom of this infection is the rash, which can last over two months. The specific cause is unknown, and it resolves on its own in several weeks’ time. No treatment is necessary, but we sometimes prescribe antifungal shampoo and oatmeal baths for comfort. It is not contagious, even to close household members. It rarely leaves scars or evidence of infection once it has cleared.

Also called hives, urticaria can present as a result of allergy, insect bite, viral infection, agitating contact, or emotional stress. In general, hives look like swollen welts on the skin, usually flesh-colored or with some redness. Diagnostically, they are non-specific and often fleeting or roaming. That means there may be a localized eruption of hives on the face, and an hour later they may have resolved with a new patch of hives showing up on the belly.
Urticaria can result from an allergic response (something touching the skin, inhaled, or ingested), a viral infection, or even a stress reaction. One reliable feature of hives is that they are intensely itchy. Regardless of trigger, hives are histamine-mediated and usually respond to antihistamines like Benadryl, Claritin, and Zyrtec. Severe cases of urticaria may require prescription antihistamines or even oral steroids to help reduce the inflammatory response. Other than avoiding a known allergen, there is no reliable way to escape urticaria, since its cause sometimes remains unknown.
 Also called “Chicken skin”, KP is commonly found on the upper arms, thighs, and cheeks. Lesions look like densely packed flesh-colored or red dots and feel like bumpy skin. It might get worse in the drier winter months but can be seen year-round. KP results when extra keratin, the cells that make up the outermost layer of the epidermis, clog the tiny hair follicles on the skin. This results in a small pimple at the hair’s base.
Also called “Chicken skin”, KP is commonly found on the upper arms, thighs, and cheeks. Lesions look like densely packed flesh-colored or red dots and feel like bumpy skin. It might get worse in the drier winter months but can be seen year-round. KP results when extra keratin, the cells that make up the outermost layer of the epidermis, clog the tiny hair follicles on the skin. This results in a small pimple at the hair’s base.
Keratosis pilaris tends to run in families. KP isn’t dangerous or contagious, and it doesn’t require intervention. It is mostly an esthetic issue but can be distressing to the patient when it flares. There is no specific cure, but the combination of gentle exfoliating with a loofah or washcloth in the shower or bath and then moisturizing afterwards often calms down an exacerbation of KP. Prescription and over-the-counter creams with lactic acid may help as well.
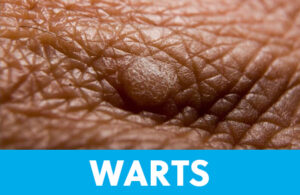
Verruca, as they are called in medical Latin, are most often found on the soles of the feet or palms of the hands. Warts feel rough and hard, and look dry. Sometimes warts have black dots at the center of the lesion. Those located on the ball of the foot can cause pain when stepping or walking. Contagious by direct or secondary contact, warts are often contracted at the pool or in a public shower. The virus that causes warts can survive on surfaces for up to 6 months, so protect yourself by wearing shower shoes or flip-flops and avoid walking barefoot.
In the office, we treat warts with a scalpel and a topical blistering agent. The scalpel removes the dead skin from the surface of the wart so that the medication can be optimally absorbed. At home, instead of a scalpel, we recommend using a pumice stone or nail file (reserved for this purpose and not used on other areas of skin) to pare down the skin that covers the wart. It is best to do this while the skin is clean and soft, so after bathing or soaking the foot. Once the wart is exposed, over-the-counter topical medications like salicylic acid can be utilized. Studies have shown that Duct tape has been used to help resolve warts as well. The skin under the tape becomes soft and when the tape is removed, the adhesive exfoliates the area, which helps uncover the wart and make it more susceptible to treatment.
Genital warts are also viral, most notably HPV (Human Papilloma Virus), a germ that can be a precursor to head, throat, penile, rectal, and cervical cancers. While plantar warts on the feet can be caused by casual contact, genital warts are a sexually transmitted illness that results from intimate contact. The American Academy of Pediatrics recommends vaccination to safeguard against contracting HPV, and studies show a complete HPV series of shots does provide robust protection.

Eczema is considered an atopic disease. Atopy refers to conditions where the body over-reacts to the environment, and includes eczema and allergies and asthma. These conditions tend to be found together if not in the same patient at least in the same family. It is not contagious; eczema is immune-mediated, meaning the body’s immune system modulates its severity. Certain predictable triggers can cause an eczema flare, including exposure to an allergen, dry skin, and infection. Eczema is often found where joints fold (known as “flexor surfaces”), like the wrist, inside bend of the elbow, behind the knee, or at the front of the ankle. Diagnostically, this helps differentiate from psoriasis, which prefers extensor surfaces of skin. Eczema, because it is an inflammatory condition, can cause color change in the skin. Mostly this is temporary, and resolves as new skin cells are generated. On the face, however, it can be distressing for the patient. When the skin looks lighter in an area of eczema, it is called hypopigmentation.
There are many sub-categories of eczema, including dishydrotic eczema (which looks like tiny pimples and can be confused with Hand Foot and Mouth), and nummular eczema (which, because it appears in discrete circular patterns, can be confused with ringworm). For the most part, eczema of any kind will respond to topical therapy. Aggressive moisturizing and avoidance of any agitating scents, dyes, or allergens will help to keep the skin smooth. When that fails, topical steroids are usually prescribed. For severe cases, oral steroids might be employed. It’s unsafe to take oral steroids long-term, and topical steroids can result in the same hypopigmentation as untreated eczema, so an alternative treatment was developed: Pimecrolimus and Tacrolimus, historically used as anti-rejection drugs in patients after organ transplant, were formulated into a topical delivery method to allow a non-invasive, non-steroid option for eczema care. Used correctly, these have broadened the safe choices available to keep eczema outbreaks at bay.

Acne, burns, abrasions, cuts, piercings, tattoos, and surgery can all leave scars. Anything that disrupts the skin can leave a permanent mark. It can take anywhere from several weeks to a year or two to determine the final appearance of a scar. Sometimes, instead of healing, the skin develops scar tissue that extends beyond the area of injury. This is called a keloid. Some patients will develop keloids, large and rubbery masses at the site where the skin barrier was broken. It can be impossible to predict who will develop keloids (though they are more common in skin with more pigment), even from what’s mostly considered benign procedures like body ink or piercing, and to what extent these masses will grow. Dermatologists and plastic surgeons can inject these lesions or surgically remove them, but every new cut risks another potential keloid.
Burn scars can appear wiry or sinewy and, if located over a joint, can interfere with that area’s range of motion. Self-inflicted injury, like cutting, can be easy to recognize in a patient with several parallel linear scars down the length of their forearm. Some patients, however, are more sly with their self-harm and it may not be located on a part of the skin that’s readily visible. Some teens and young adults don’t cut, but instead burn themselves. A recent Tik-Tok dared watchers to spray aerosolized deodorant on their skin at close range and see how long they could tolerate the pain. This creates thermal injury that will cause skin necrosis and scarring, and possibly infection.
Health care practitioners, teachers and day care workers, social workers, therapists, foster parents, and attorneys are among those in Ohio that are considered mandated reporters. These individuals are required by law to report if known or suspected child abuse is occurring. Scars can be difficult to interpret but can raise a red flag for non-accidental injury. While there are entire books and seminars on how to recognize child abuse and laypeople are not expected to be experts, if there is even a suspicion that a minor is being victimized, concerns should be properly addressed.
While healing, topical antibiotic ointment gently massaged on the wound can help minimize the appearance of scarring and the development of scar tissue under the skin. Once the skin is healed, topical application of vitamin E oil or gel can help diminish the appearance of a non-keloid scar.
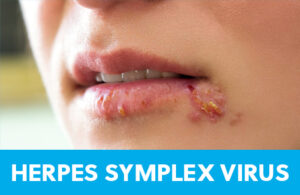
HSV is the family of virus responsible for cold sores, chicken pox, shingles, and genital Herpes. While the great majority of people worldwide have antibodies against HSV, these do not provide a guaranteed defense against infection. Prior to 1995, when the US made a chicken pox (varicella) vaccine available, almost all children got infected by age ten. Before vaccination, we saw more than four million cases of chicken pox, at least 10,000 hospitalizations for varicella-related illnesses like meningitis and pneumonia, and up to 150 deaths every year in children. These days, since schools mandate varicella vaccine for attendance, we don’t see this morbidity and mortality anymore.
Whether immunity is gained through active chicken pox infection or through live vaccination, the germ remains dormant in the body’s nervous system for years. Re-activation of chicken pox (varicella) is called shingles, and typically presents as a tingling that precedes a painful blistering rash, often in a linear distribution over half of the torso. Unlike chicken pox, which is quite contagious, shingles does not spread easily from one person to the next. Also unlike a chicken pox infection that usually comes with a fever, muscle aches, and cold symptoms, a shingles infection is usually limited to just the uncomfortable rash. Shingles often occurs when the body’s system is stressed, either through illness, pregnancy, exhaustion, or emotional strain. Acyclovir is the prescription antiviral that is used to help shorten the course and diminish the severity of a shingles infection.
HSV is also responsible for cold sores, also known as fever blisters. Like shingles, this is a reactivation of virus that occurs when the body is in a stressed state, often with a viral cold or fever, as their names suggest. In medical-ese, we call these lesions herpes labialis, and they present, like shingles, with a tingle that precedes any visible rash. After the tingle, there is a blister-like lesion usually at the lip’s border, which eventually, like chicken pox and shingles, scabs over once it’s no longer contagious. Topical antivirals are available to help these lesions heal faster, and should be started at the very first sensation of tingling.
Genital herpes is a lifelong condition that will periodically flare up with painful lesions in sensitive areas. It is considered a sexually transmitted disease. Valacyclovir is a daily prescription for patients with genital herpes that reduces the number and frequency of outbreaks and saves infants from exposure during delivery.

People sometimes confuse Scarlet fever and Rheumatic fever. Scarlet fever is what doctors call it when a patient has a fever, a positive strep test, and a pink, dotty rash on the torso. Rheumatic fever is a serious heart condition that can occur if strep throat is not treated with antibiotics, so it’s a rare occurrence in modern day. The textbook rash that can accompany a strep throat infection is described as “sandpapery”. It feels rough and dry, and the lesions are densely packed, especially in the warmer pockets of the armpits and groin. While it can be seen on the arms, scarlatina (strep rash) is often found in a vest-like distribution. Scarlet fever is no more dangerous than a strep throat infection without a rash. Strep throat is contagious through droplets like sneezing, coughing, and sharing drinks. Most strep infections are sensitive to Amoxicillin, and as long as the fever has resolved, patients can usually get back to work or school once they’ve been on antibiotics for at least 24 hours. The incubation period for strep throat is typically 2-4 days, and patients may complain of headache, fever, difficulty swallowing, and swollen lymph nodes, in addition to rash and sore throat. Like most rashes, even after it fades, you may notice it again for a couple of weeks when the patient is warm, say from snuggling in bed overnight, taking a shower or bath, or vigorously exercising. Brief re-emergence of this rash does not necessarily indicate re-infection.

A common childhood rash, Molluscum’s contagious nature is built right into its name. Molluscum is caused by a Poxvirus that is easily passed from one patient to another through skin-to-skin contact. It can also live in water and on soft surfaces, so children with Molluscum should not share bath towels with siblings. These lesions are typically rounded with a central divot. They appear in crops, often on surfaces of skin that communicate, like the inner thighs, or the bicep area and the lateral torso. The natural history of Molluscum is that the rash usually resolves on its own, but can take anywhere from 6 months to 5 years to clear. And in that span of time, it often gets transferred to another body part or another person altogether. Because this virus belongs to the same family of germ that causes warts, sometimes the same therapies are employed. Cryotherapy (freezing) has demonstrated moderate success, and “unroofing” the lesion in a doctor’s office, while not pretty, will eliminate lesions from the skin. Imiquimod is a prescription agent that can be applied sparingly to Molluscum lesions to help hasten resolution as well.
From UH Pediatrician and PSI Medical Expert – Dr. Carly Wilbur.
Click here for more great insights from Dr. Wilbur.

Leave A Comment
You must be <a href="https://www.psi-solutions.org/wp-login.php?redirect_to=https%3A%2F%2Fwww.psi-solutions.org%2Fthe-skin-youre-in%2F">logged in</a> to post a comment.